Living with lymphedema can feel like managing two problems at once: the visible swelling and the daily routine needed to keep it under control. While compression garments, massage, and exercise remain essential, some patients still experience progressive heaviness, recurring infections, and reduced mobility. In these cases, reconstructive techniques at Liv Hospital can offer a more targeted approach by addressing how lymph fluid is (or isn’t) moving through the body.
What Is Lymphedema and Why Does It Become Chronic?
Lymphedema occurs when the lymphatic system cannot drain lymph fluid effectively. That fluid is protein-rich, which matters because protein attracts inflammation. Over time, the affected limb can shift from “soft and puffy” swelling to a firmer, heavier condition where the skin and deeper tissues thicken.
Common triggers include:
- Cancer treatment that removes or damages lymph nodes (for example breast, gynecologic, or melanoma surgery)
- Radiation therapy that scars lymph channels
- Inherited lymphatic malformations (primary lymphedema)
- Trauma, infection, or repeated inflammation that disrupts drainage pathways
Early lymphedema may improve with elevation and compression. Long-standing lymphedema can become more resistant because fluid stasis eventually leads to fat deposition and fibrosis (scar-like tissue), making the swelling partly “solid,” not just fluid.
The Two Main Goals of Surgery: Drain Better or Reduce Volume
Modern lymphedema surgery generally follows one (or both) of these strategies:
1) Physiologic repair (improving drainage)
This category focuses on restoring flow—helping lymph find a new route around a blockage or rebuilding lymph function in the affected area.
2) Volume reduction (removing chronic tissue changes)
This category focuses on reducing the bulk created by long-term inflammation, where excess fatty and fibrotic tissue becomes part of the problem.
The best approach depends on what’s driving the swelling: fluid dominance (earlier stages) vs. solid tissue dominance (later stages).
Physiologic Options: Rebuilding Drainage PathwaysLymphaticovenous Anastomosis (LVA)
LVA is a super-microsurgical technique where tiny lymphatic vessels are connected to nearby small veins. Think of it as creating a “new exit route” so lymph fluid can bypass damaged areas and drain into the venous system.
LVA tends to be most helpful when:
- Swelling is still soft or pitting
- Lymphatic channels still have some function
- The goal is to reduce heaviness and lower infection risk
Because the incisions are small and the work is delicate, recovery is often easier than major excisional surgery, but results depend heavily on staging and vessel quality.
Vascularized Lymph Node Transfer (VLNT)
VLNT involves transferring healthy lymph nodes (with their blood supply) from one part of the body to the affected region. These nodes can help absorb fluid and may encourage the body to form new lymphatic connections over time.
VLNT may be considered when:
- Lymph nodes were removed during cancer treatment
- Imaging shows poor lymphatic function in the affected area
- Swelling is persistent despite consistent conservative therapy
Surgeons plan donor sites carefully to reduce the risk of causing swelling in the donor area.
Volume-Reduction Options: When Tissue Has HardenedSuction-Assisted Protein Lipectomy (SAPL)
In advanced lymphedema, the limb can enlarge not just from fluid, but from lymphedema-related fat growth and fibrosis. SAPL is a specialized form of liposuction designed to remove that disease-altered tissue and reduce limb size.
This is different from cosmetic liposuction because:
- The goal is medical symmetry and functional improvement
- Technique prioritizes the remaining lymphatic structures
- Long-term compression is usually still needed afterward
SAPL can be life-changing for patients with non-pitting, fibrotic swelling where drainage procedures alone won’t meaningfully reduce size.
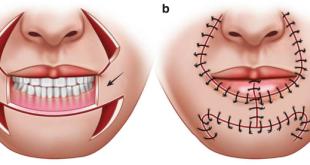
Excisional Procedures (for severe end-stage cases)
In extreme cases with severe skin changes, recurrent infections, and disabling enlargement, excisional surgery may be considered. These procedures remove thickened tissue and may require skin grafting. They are typically reserved for advanced disease when other options cannot provide enough improvement.
Why Imaging and Staging Decide Everything
Lymphedema is not “one type of swelling,” so accurate assessment is critical. Clinics often use imaging such as ICG lymphography or other mapping tools to evaluate lymphatic pathways and determine whether the condition is more fluid-based or solid-based.
This evaluation helps answer practical questions like:
- Are there functional lymphatic vessels suitable for LVA?
- Would VLNT provide meaningful regeneration potential?
- Is the bulk mostly fibrotic tissue that needs debulking first?
- Which plan offers the most realistic reduction in infections and heaviness?
What Patients Often Notice After Successful Treatment
While results vary, many patients pursue surgery to reduce the daily burden of lymphedema—not necessarily to erase it completely. Improvements often focus on:
- Less heaviness and fatigue in the limb
- Better mobility and easier walking or arm use
- Fewer episodes of cellulitis and skin inflammation
- Easier fit of clothing and improved body confidence
- Reduced reliance on intensive daily therapy routines
If you want to read the clinical overview in one place, PLASTIC SURGERY Lymphedema Surgery explains the topic in detail.
Long-Term Success Still Depends on Daily Habits
Even after surgery, lymphedema is usually managed as a long-term condition. Ongoing compression (sometimes reduced), skin care, movement, and weight stability remain important for keeping swelling controlled and preventing infection. Many patients find it helpful to build sustainable wellness routines—sleep, nutrition, and stress reduction—because these factors influence inflammation and recovery, and resources like live and feel can support those lifestyle habits in a practical way.
 Pagal World
Pagal World